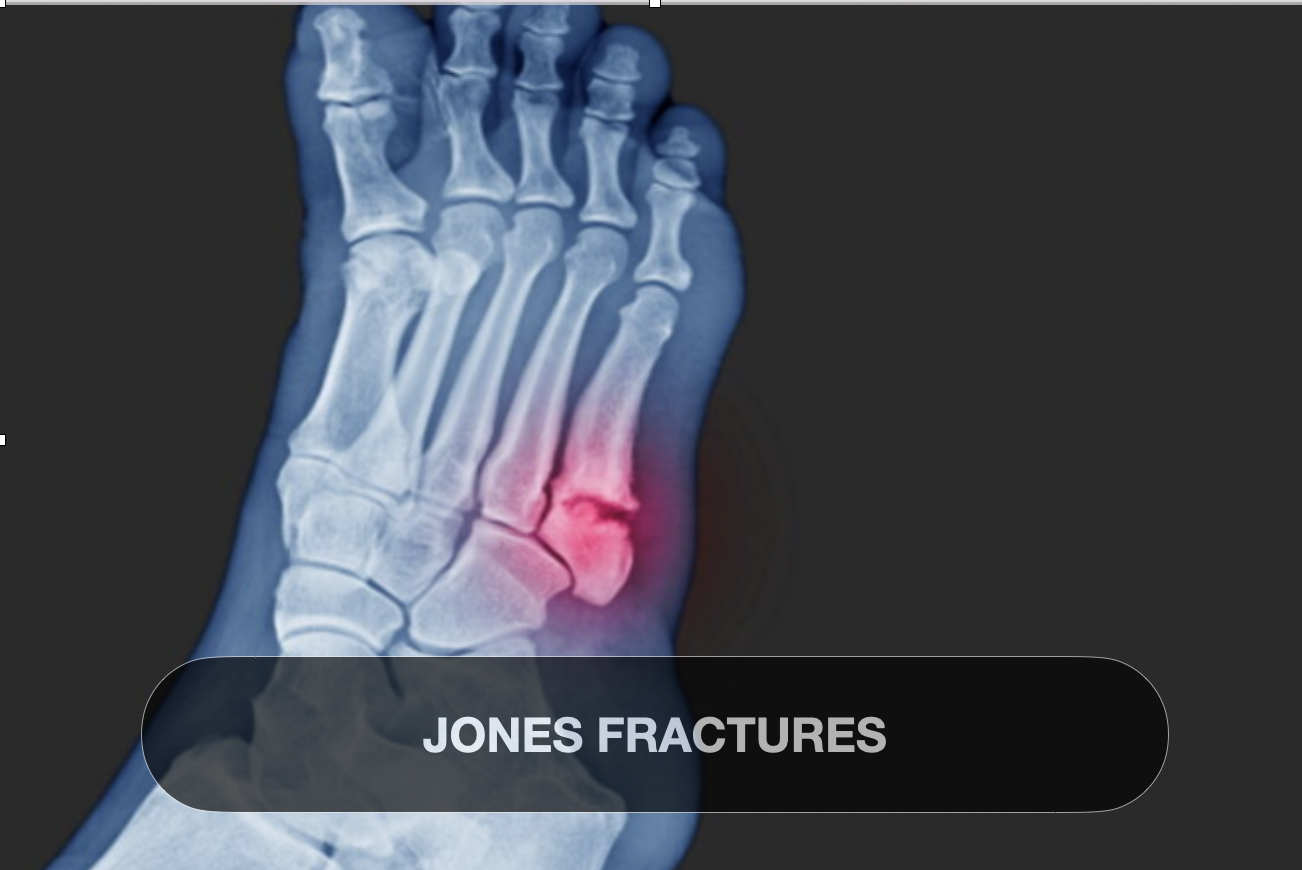
JONES FRACTURES
Jones fractures
🦶 Introduction
A Jones fracture is a distinct type of break in the fifth metatarsal, located at the metaphyseal-diaphyseal junction—approximately 1.5–3 cm from the base of the bone. First described by Sir Robert Jones in 1902, it remains clinically significant due to its tendency for poor healing, delayed union, or nonunion owing to limited blood supply in the region. This injury is especially relevant to physically active populations—athletes, dancers, military personnel—as well as older adults, given its association with high-impact, torsional movements and compromised bone. Treatment must be tailored, balancing fracture stability, patient activity level, and mitigation of complications.
✅ Structured Scientific Summary
1. Definition
A Jones fracture occurs at the proximal 5th metatarsal metaphyseal-diaphyseal junction (Zone 2), distinct from avulsion or stress fractures
Characterized by its high risk of delayed union or nonunion, due to its anatomical vascular watershed location
2. Cause
Acute torsional trauma: Inversion of the foot with the toe pointed, common in basketball, dancing, football, or slips and falls
Repetitive stress from running, jumping, and sudden direction changes
Overuse, biomechanical abnormalities (e.g., high arches), and bone density issues can predispose individuals
3. Classification
Anatomically divided into:
Zone 1: Avulsion fractures (pseudo-Jones/dancer’s).
Zone 2: True Jones fractures (metaphyseal-diaphyseal junction).
Zone 3: Proximal stress fractures
Clinical importance lies in differentiating Jones (Zone 2) from other zones due to varied healing outcomes and management strategies
4. Signs & Symptoms
Pain: Acute, sharp, lateral midfoot pain, worsened by weight-bearing
Tenderness and focal swelling/bruising over the fifth metatarsal base
Difficulty or inability to bear weight; may present as a limp
Chronic residual symptoms: persistent pain or instability if left untreated or mismanaged
Diagnosis confirmed via multi-view X-rays; sometimes CT/MRI to assess nonunion risk
5. Current Treatment Trends
A. Non-surgical management
Immobilisation: Non-weight-bearing cast or boot for 6–8 weeks; potentially extended to 12 weeks if healing is delayed
Adjunct modalities: NSAIDs, ice, elevation, and low-intensity bone stimulation to support healing
Physical therapy post-immobilisation focuses on range of motion, strength, proprioception, gait correction, and gradually reintroducing functional load—typically over 3–4 months
B. Surgical intervention
Indications: Displaced fractures (>2–3 mm), high-performance athlete, early union failure, or early return-to-play goals
Fixation: Intramedullary screw (often cannulated), sometimes with plates/allograft in nonunion cases
Outcomes: Surgical fixation accelerates healing, with radiographic union in ~97% compared to ~79% in conservative cases
Accelerated rehab protocols: Early protected weight-bearing in boot (0–2 weeks), progressive ROM/strengthening (2–6 weeks), sport-specific drills by 8–12 weeks, full return ~12 weeks
6. Prognosis & Challenges
Nonunion rates for conservatively managed Jones fractures range from 21–50%, whereas surgically managed cases demonstrate ~97% union
Risk factors: poor vascular supply, biomechanical stress, comorbidities (e.g., osteoporosis)
Surgical risks: hardware complications, infection, refracture—though many athletes resume sports within ~8 weeks under accelerated protocols
🏥 Clinical Implications
Early Detection: Recognise Zone 2 injuries via focal lateral foot pain and targeted palpation.
Active Rehab: Implement progressive protocols: begin with joint mobilities, then progress balance and functional drills, up to plyometrics and sport movements.
Collaborative Decision-Making: Consider patient’s activity demands; involve surgeons early when fracture displacement or nonunion risk is high.
Guided Return-To-Play: Use time-based, milestone-driven plans (e.g., 8–12 week goal for athletes).
Monitor Complications: Observe for nonunion signs; advocate for imaging if symptoms persist beyond expected healing window.